Thyroid Diseases
Overview
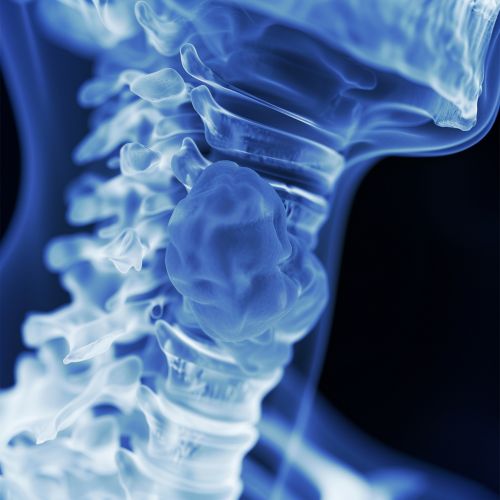
Thyroid diseases encompass a range of disorders that affect the thyroid gland, a butterfly-shaped endocrine gland located in the neck. The thyroid gland plays a crucial role in regulating metabolism, growth, and development through the production of thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3). Dysfunctions in the thyroid gland can lead to various clinical conditions, broadly categorized into hyperthyroidism, hypothyroidism, thyroiditis, thyroid nodules, and thyroid cancer.
Anatomy and Physiology of the Thyroid Gland
The thyroid gland is situated anteriorly in the neck, below the larynx, and consists of two lobes connected by an isthmus. It is richly supplied with blood vessels and innervated by the autonomic nervous system. The gland synthesizes thyroid hormones by absorbing iodine from the bloodstream and combining it with the amino acid tyrosine. The hypothalamus and pituitary gland regulate thyroid function through the release of thyrotropin-releasing hormone (TRH) and thyroid-stimulating hormone (TSH), respectively.
Hyperthyroidism
Hyperthyroidism is characterized by excessive production of thyroid hormones, leading to an accelerated metabolic state. Common causes include Graves' disease, toxic multinodular goiter, and thyroiditis. Symptoms of hyperthyroidism include weight loss, heat intolerance, palpitations, and nervousness. Diagnosis is confirmed through elevated levels of free T4 and T3, and suppressed TSH levels. Treatment options include antithyroid medications, radioactive iodine therapy, and thyroidectomy.
Graves' Disease
Graves' disease is an autoimmune disorder where autoantibodies stimulate the TSH receptor, causing hyperthyroidism. It is often associated with ophthalmopathy and dermopathy. The condition is diagnosed through clinical presentation, thyroid function tests, and the presence of thyroid-stimulating immunoglobulins (TSI). Management includes antithyroid drugs, radioactive iodine, and surgical intervention in refractory cases.
Hypothyroidism
Hypothyroidism results from insufficient production of thyroid hormones, leading to a slowed metabolic rate. Primary hypothyroidism is commonly due to Hashimoto's thyroiditis, iodine deficiency, or iatrogenic causes. Symptoms include fatigue, weight gain, cold intolerance, and depression. Diagnosis involves elevated TSH levels and low free T4 levels. Treatment primarily consists of levothyroxine replacement therapy.
Hashimoto's Thyroiditis
Hashimoto's thyroiditis is an autoimmune disorder characterized by lymphocytic infiltration and destruction of thyroid tissue. It is the most common cause of hypothyroidism in iodine-sufficient regions. The presence of anti-thyroid peroxidase (anti-TPO) and anti-thyroglobulin antibodies confirms the diagnosis. Long-term management includes monitoring thyroid function and adjusting levothyroxine dosage.
Thyroiditis
Thyroiditis refers to inflammation of the thyroid gland and can be classified into several types, including acute, subacute, and chronic thyroiditis. Subacute thyroiditis, also known as De Quervain's thyroiditis, is often viral in origin and presents with a painful, enlarged thyroid gland and systemic symptoms. Chronic thyroiditis, such as Hashimoto's, is autoimmune in nature. Treatment varies based on the type and severity of inflammation.
Thyroid Nodules
Thyroid nodules are discrete lesions within the thyroid gland that may be benign or malignant. They are often discovered incidentally during imaging studies or physical examination. Fine-needle aspiration (FNA) biopsy is the gold standard for evaluating the nature of thyroid nodules. Benign nodules may require observation, while malignant or suspicious nodules necessitate surgical excision.

Thyroid Cancer
Thyroid cancer arises from the follicular or parafollicular cells of the thyroid gland. The most common types include papillary, follicular, medullary, and anaplastic thyroid cancer. Papillary thyroid cancer is the most prevalent and has a favorable prognosis. Diagnosis is based on cytological evaluation from FNA biopsy, imaging studies, and serum markers such as calcitonin for medullary thyroid cancer. Treatment involves surgical resection, radioactive iodine therapy, and thyroid hormone suppression therapy.
Diagnosis and Management
The diagnosis of thyroid diseases involves a combination of clinical evaluation, laboratory tests, and imaging studies. Serum TSH, free T4, and T3 levels are fundamental in assessing thyroid function. Imaging modalities such as ultrasound, radioactive iodine uptake scans, and fine-needle aspiration biopsy play a crucial role in the evaluation of thyroid nodules and cancer. Management strategies are tailored to the specific disorder and may include pharmacotherapy, radioactive iodine, and surgical interventions.
