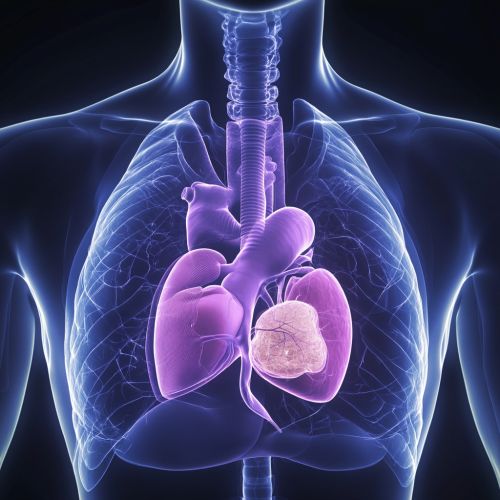
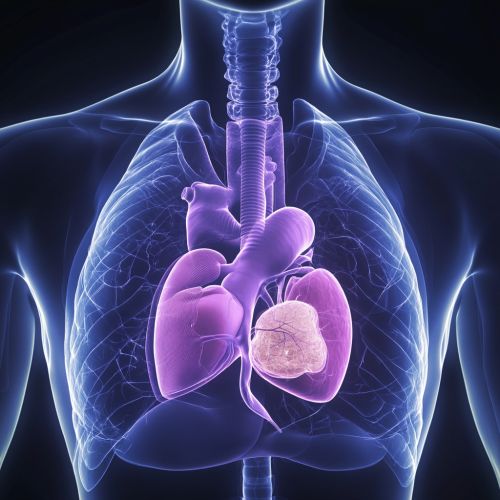
Thymus
Anatomy and Physiology of the Thymus
The thymus is a specialized primary lymphoid organ of the immune system. Located in the anterior superior mediastinum, in front of the heart and behind the sternum, the thymus plays a critical role in the development and maturation of T-lymphocytes (T cells), which are essential for adaptive immunity.
Structure
The thymus is composed of two identical lobes and is divided into an outer cortex and an inner medulla. The cortex is densely packed with immature T cells (thymocytes), while the medulla contains fewer, more mature thymocytes. The thymus is encapsulated by a connective tissue capsule that extends inward to form septa, dividing the lobes into lobules.
The thymic stroma consists of epithelial cells, which form a three-dimensional network that supports the developing thymocytes. The epithelial cells in the cortex are known as cortical thymic epithelial cells (cTECs), and those in the medulla are called medullary thymic epithelial cells (mTECs). These cells play a crucial role in the positive and negative selection of T cells, ensuring that only functional and self-tolerant T cells are released into the peripheral blood circulation.
Development
The thymus originates from the third pharyngeal pouch during embryogenesis. It is fully developed at birth and reaches its maximum size during puberty. After puberty, the thymus undergoes a process called involution, where it gradually decreases in size and becomes replaced by adipose tissue. Despite this reduction in size, the thymus continues to produce T cells throughout an individual's life, albeit at a reduced rate.
Function
The primary function of the thymus is to generate a diverse and self-tolerant T cell repertoire. This process involves several stages:
1. **T Cell Progenitor Migration**: Hematopoietic stem cells from the bone marrow migrate to the thymus, where they differentiate into thymocytes. 2. **Positive Selection**: In the cortex, thymocytes expressing T cell receptors (TCRs) that can recognize self-major histocompatibility complex (MHC) molecules are selected for survival. This ensures that T cells can interact with MHC molecules, which present antigens to T cells. 3. **Negative Selection**: In the medulla, thymocytes that strongly bind to self-antigens presented by mTECs undergo apoptosis. This process eliminates potentially autoreactive T cells, preventing autoimmune diseases. 4. **Maturation and Release**: Surviving thymocytes mature into functional T cells and are released into the bloodstream to perform immune surveillance and response.
Clinical Significance
Thymic Disorders
Several disorders can affect the thymus, impacting its function and leading to immune deficiencies or autoimmune diseases.
Thymic Hyperplasia
Thymic hyperplasia refers to an enlargement of the thymus, which can be associated with conditions such as myasthenia gravis, Graves' disease, and systemic lupus erythematosus. In myasthenia gravis, thymic hyperplasia is often accompanied by the presence of germinal centers, which are sites of active B cell proliferation.
Thymoma
Thymoma is a neoplasm arising from the epithelial cells of the thymus. It is the most common tumor of the anterior mediastinum and can be associated with paraneoplastic syndromes, such as myasthenia gravis. Thymomas are classified into different types based on their histological appearance and behavior, ranging from benign to highly malignant thymic carcinoma.
DiGeorge Syndrome
DiGeorge syndrome, also known as 22q11.2 deletion syndrome, is a genetic disorder characterized by the congenital absence or hypoplasia of the thymus. This results in a severe T cell deficiency, leading to increased susceptibility to infections. Patients with DiGeorge syndrome may also have cardiac anomalies, hypocalcemia, and facial dysmorphisms.
Thymectomy
Thymectomy, the surgical removal of the thymus, is performed in certain medical conditions. It is a standard treatment for myasthenia gravis, particularly in patients with thymomas. Thymectomy can also be performed in cases of thymic hyperplasia or other thymic tumors. The procedure can be done via open surgery or minimally invasive techniques, such as video-assisted thoracoscopic surgery (VATS).
Thymic Involution and Aging
The process of thymic involution, where the thymus decreases in size and function with age, has significant implications for the immune system. As the thymus involutes, the production of new T cells declines, leading to a reduced immune response in older adults. This contributes to increased susceptibility to infections, a higher incidence of cancer, and a diminished response to vaccinations in the elderly.
Research into reversing or slowing thymic involution is ongoing, with potential therapies including cytokine administration, hormonal treatments, and regenerative medicine approaches. Understanding the mechanisms of thymic involution and developing strategies to maintain thymic function are critical for improving immune health in aging populations.
Thymic Hormones
The thymus produces several hormones that play a role in T cell development and function. These include thymosin, thymopoietin, and thymulin. Thymosin, a peptide hormone, is involved in the differentiation and maturation of T cells. Thymopoietin influences the migration and differentiation of thymocytes, while thymulin enhances T cell function and modulates the immune response.
The production of thymic hormones declines with age, contributing to the reduced immune function observed in older individuals. Supplementation with thymic hormones or their analogs is being explored as a potential therapeutic approach to enhance immune function in immunocompromised patients and the elderly.
Thymic Microenvironment
The thymic microenvironment is crucial for the proper development and selection of T cells. It consists of various cell types, including thymic epithelial cells, dendritic cells, macrophages, and fibroblasts. These cells interact with developing thymocytes through cell-cell contact and the secretion of cytokines and growth factors.
Dendritic cells and macrophages in the thymus present antigens to thymocytes, facilitating the process of negative selection. The thymic epithelial cells provide structural support and produce cytokines, such as interleukin-7 (IL-7), which are essential for thymocyte survival and proliferation.
The extracellular matrix (ECM) within the thymus also plays a role in T cell development. The ECM components, such as fibronectin, laminin, and collagen, provide a scaffold for thymocyte migration and influence their differentiation through signaling pathways.
Thymic Regeneration
Thymic regeneration is the process by which the thymus restores its structure and function after injury or atrophy. This can occur naturally, such as during recovery from stress or infection, or can be induced through therapeutic interventions.
Several strategies are being investigated to promote thymic regeneration, including:
1. **Cytokine Therapy**: Administration of cytokines, such as IL-7 and keratinocyte growth factor (KGF), has been shown to enhance thymic regeneration and improve T cell output. 2. **Stem Cell Therapy**: Transplantation of hematopoietic stem cells or thymic epithelial progenitor cells holds promise for regenerating the thymic microenvironment and restoring T cell production. 3. **Hormonal Therapy**: Hormones, such as growth hormone and sex steroids, have been studied for their potential to stimulate thymic regeneration and counteract thymic involution.
Understanding the mechanisms underlying thymic regeneration and developing effective therapies are important for improving immune function in patients with thymic atrophy or damage.
