Pulmonary alveoli
Structure and Function of Pulmonary Alveoli
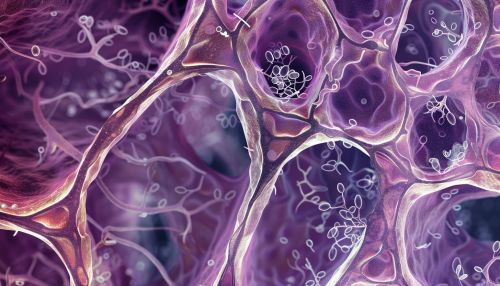
Pulmonary alveoli are the microscopic air sacs located at the terminal ends of the respiratory tree, and they are the primary sites for the exchange of gases between the air and the blood. Each human lung contains approximately 300 million alveoli, which collectively provide a vast surface area of about 70 square meters for gas exchange. This extensive surface area is crucial for efficient oxygen uptake and carbon dioxide removal.
Anatomy
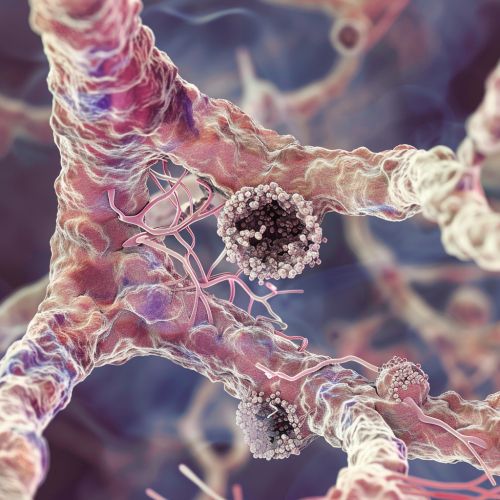
The alveoli are clustered in grape-like formations known as alveolar sacs. Each alveolus is a small, balloon-like structure with a thin wall composed of a single layer of epithelial cells. These cells are primarily of two types: Type I and Type II alveolar cells. Type I cells, also known as squamous alveolar cells, cover about 95% of the alveolar surface and are involved in the process of gas exchange. Type II cells, or great alveolar cells, secrete surfactant, a substance that reduces surface tension within the alveoli, preventing their collapse during exhalation.
The alveolar walls are richly supplied with a network of capillaries, which are essential for the exchange of gases. The close proximity of the alveolar epithelium and the capillary endothelium forms the respiratory membrane, which is only about 0.5 micrometers thick. This thin barrier facilitates the rapid diffusion of oxygen and carbon dioxide.
Physiology
The primary function of the pulmonary alveoli is to facilitate the exchange of gases between the air and the blood. This process is driven by differences in partial pressures of oxygen and carbon dioxide across the respiratory membrane. Oxygen from the inhaled air diffuses through the alveolar walls and into the blood in the capillaries, while carbon dioxide from the blood diffuses into the alveoli to be exhaled.
The efficiency of gas exchange is influenced by several factors, including the surface area of the alveoli, the thickness of the respiratory membrane, and the partial pressure gradients of the gases. Conditions such as pulmonary fibrosis can thicken the respiratory membrane, reducing the efficiency of gas exchange.
Surfactant
Surfactant is a lipoprotein complex secreted by Type II alveolar cells. It plays a critical role in maintaining alveolar stability by reducing surface tension. Without surfactant, the alveoli would be prone to collapse, especially during exhalation when the alveolar volume decreases. Surfactant also helps to keep the alveoli dry by preventing the transudation of fluid from the capillaries into the alveolar spaces.
The production of surfactant begins late in fetal development, and insufficient surfactant production in premature infants can lead to neonatal respiratory distress syndrome.
Blood-Air Barrier
The blood-air barrier, also known as the respiratory membrane, is composed of the alveolar epithelial cells, the capillary endothelial cells, and their fused basement membranes. This barrier is extremely thin, allowing for the efficient diffusion of gases. The integrity of the blood-air barrier is crucial for proper lung function, and any damage to this barrier can lead to pulmonary edema and impaired gas exchange.
Pathophysiology
Several diseases and conditions can affect the structure and function of the pulmonary alveoli. Chronic obstructive pulmonary disease (COPD) is characterized by the destruction of alveolar walls, leading to a decrease in the surface area available for gas exchange. Emphysema, a type of COPD, involves the permanent enlargement of the alveoli and loss of elastic recoil, which impairs the ability to expel air from the lungs.
Pulmonary edema occurs when fluid accumulates in the alveoli, reducing the surface area for gas exchange and leading to respiratory distress. This condition can be caused by heart failure, acute respiratory distress syndrome (ARDS), or exposure to toxins.
Regeneration and Repair
The alveoli have a limited capacity for regeneration and repair. Type II alveolar cells can proliferate and differentiate into Type I cells to replace damaged epithelium. However, extensive damage to the alveoli, as seen in conditions like idiopathic pulmonary fibrosis, can lead to scarring and permanent loss of function.
Research and Advances
Recent research has focused on understanding the molecular mechanisms underlying alveolar development, repair, and regeneration. Studies on stem cells and tissue engineering hold promise for developing new treatments for lung diseases that affect the alveoli. Advances in imaging techniques, such as high-resolution computed tomography (HRCT), have improved the ability to diagnose and monitor alveolar pathology.
See Also
- Respiratory system
- Gas exchange
- Chronic obstructive pulmonary disease
- Pulmonary fibrosis
- Neonatal respiratory distress syndrome
- Pulmonary edema
- Stem cell therapy
