Osteoclasts
Introduction
Osteoclasts are specialized multinucleated cells that play a crucial role in bone resorption, a process essential for the maintenance, repair, and remodeling of bones. These cells are derived from hematopoietic stem cells and are part of the monocyte-macrophage lineage. Osteoclasts are responsible for breaking down bone tissue by secreting acids and enzymes that dissolve the mineralized matrix and collagen. This process is vital for calcium homeostasis and the continual renewal of the skeletal system.
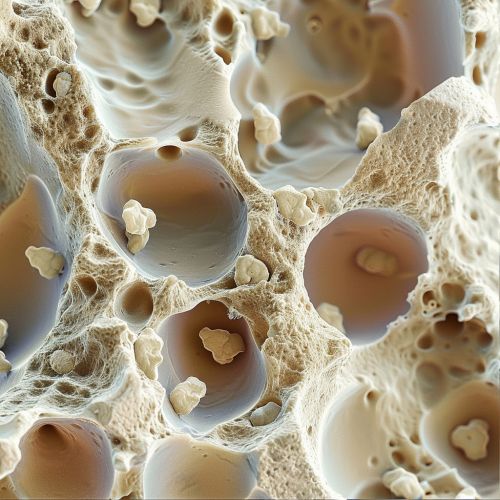
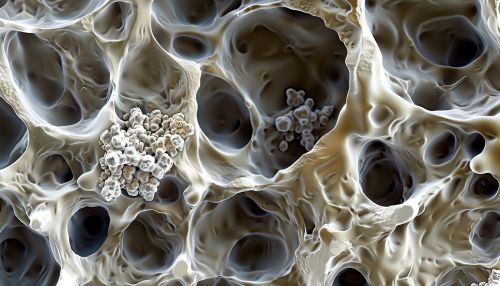
Structure and Formation
Osteoclasts are large, multinucleated cells that can contain up to 20 nuclei. They are characterized by their ruffled border, which increases the surface area for bone resorption. The formation of osteoclasts, known as osteoclastogenesis, involves several stages:
Hematopoietic Stem Cells
Osteoclasts originate from hematopoietic stem cells, which also give rise to other blood cells. These stem cells differentiate into monocyte/macrophage precursor cells under the influence of specific growth factors and cytokines.
Monocyte/Macrophage Precursors
The precursor cells further differentiate into pre-osteoclasts. This differentiation is regulated by macrophage colony-stimulating factor (M-CSF) and receptor activator of nuclear factor kappa-Β ligand (RANKL).
Fusion into Multinucleated Cells
Pre-osteoclasts fuse to form multinucleated osteoclasts. This fusion is a critical step and is influenced by factors such as dendritic cell-specific transmembrane protein (DC-STAMP) and osteoclast stimulatory transmembrane protein (OC-STAMP).
Maturation
The final stage involves the maturation of osteoclasts, where they develop a ruffled border and become fully functional. This maturation is regulated by various signaling pathways, including the RANK/RANKL/osteoprotegerin (OPG) pathway.
Function
Osteoclasts are primarily responsible for bone resorption, a process that involves the breakdown of bone tissue. This function is essential for various physiological processes:
Bone Remodeling
Bone remodeling is a continuous process where old bone tissue is replaced by new bone tissue. Osteoclasts resorb bone, creating small cavities that are later filled by osteoblasts, which form new bone. This balance between bone resorption and formation is crucial for maintaining bone strength and integrity.
Calcium Homeostasis
Osteoclasts play a vital role in regulating calcium levels in the blood. When blood calcium levels are low, osteoclast activity increases, leading to the release of calcium from the bone into the bloodstream. This process is regulated by parathyroid hormone (PTH) and calcitonin.
Bone Repair
In the event of bone injury or fracture, osteoclasts resorb the damaged bone tissue, allowing osteoblasts to form new bone. This coordinated activity ensures proper healing and restoration of bone function.
Regulation of Osteoclast Activity
The activity of osteoclasts is tightly regulated by various factors to ensure bone homeostasis:
RANK/RANKL/OPG Pathway
The RANK/RANKL/OPG pathway is a key regulator of osteoclast differentiation and activity. RANKL, expressed by osteoblasts and stromal cells, binds to RANK on the surface of osteoclast precursors, promoting their differentiation and activation. OPG, a decoy receptor for RANKL, inhibits this interaction, thereby reducing osteoclast activity.
Hormonal Regulation
Hormones such as PTH, calcitonin, and estrogen significantly influence osteoclast activity. PTH increases osteoclast activity to raise blood calcium levels, while calcitonin inhibits osteoclast function. Estrogen deficiency, as seen in postmenopausal women, leads to increased osteoclast activity and bone resorption, contributing to osteoporosis.
Cytokines and Growth Factors
Various cytokines and growth factors, including interleukins (IL-1, IL-6), tumor necrosis factor-alpha (TNF-α), and transforming growth factor-beta (TGF-β), modulate osteoclast activity. These molecules can either promote or inhibit osteoclastogenesis and bone resorption, depending on the context.
Pathological Conditions
Dysregulation of osteoclast activity can lead to several bone disorders:
Osteoporosis
Osteoporosis is characterized by decreased bone mass and increased fracture risk. It is often associated with increased osteoclast activity, leading to excessive bone resorption. This condition is prevalent in postmenopausal women due to estrogen deficiency.
Paget's Disease of Bone
Paget's disease involves abnormal bone remodeling, with increased osteoclast activity followed by disorganized bone formation. This results in enlarged and weakened bones, leading to pain, deformities, and fractures.
Osteopetrosis
Osteopetrosis, also known as marble bone disease, is a rare genetic disorder characterized by defective osteoclast function, leading to impaired bone resorption. This results in overly dense but brittle bones, causing frequent fractures and other complications.
Rheumatoid Arthritis
In rheumatoid arthritis, chronic inflammation leads to increased osteoclast activity and bone erosion, particularly in the joints. This contributes to joint deformities and functional impairment.
Therapeutic Interventions
Several therapeutic strategies target osteoclasts to treat bone disorders:
Bisphosphonates
Bisphosphonates are a class of drugs that inhibit osteoclast-mediated bone resorption. They are commonly used to treat osteoporosis and other conditions involving excessive bone loss.
Denosumab
Denosumab is a monoclonal antibody that binds to RANKL, preventing its interaction with RANK and thereby inhibiting osteoclast formation and activity. It is used to treat osteoporosis and bone metastases.
Hormone Replacement Therapy
Hormone replacement therapy (HRT) involves the administration of estrogen to reduce osteoclast activity and bone resorption in postmenopausal women. However, HRT is associated with potential risks and side effects.
Calcitonin
Calcitonin is a hormone that directly inhibits osteoclast activity. It is used in the treatment of osteoporosis and Paget's disease, although its use has declined due to the availability of more effective treatments.
Research and Future Directions
Ongoing research aims to further understand osteoclast biology and develop novel therapeutic approaches:
Molecular Mechanisms
Research is focused on elucidating the molecular mechanisms underlying osteoclast differentiation and function. This includes studying signaling pathways, transcription factors, and epigenetic regulation.
Targeted Therapies
The development of targeted therapies that specifically inhibit osteoclast activity without affecting other cell types is a major area of interest. This includes the use of small molecules, monoclonal antibodies, and gene therapy.
Biomarkers
Identifying biomarkers for osteoclast activity and bone resorption can aid in the early diagnosis and monitoring of bone diseases. This includes the use of serum and urine markers, as well as imaging techniques.
