Ossification
Introduction
Ossification, also known as osteogenesis, is the process by which new bone tissue is formed. This complex physiological process is essential for the growth, maintenance, and repair of bones. Ossification occurs through two primary mechanisms: intramembranous ossification and endochondral ossification. Both processes are crucial for the development of the skeletal system and involve a series of cellular and molecular events that result in the formation of mineralized bone matrix.
Types of Ossification
Intramembranous Ossification
Intramembranous ossification is the process by which flat bones, such as those of the skull, clavicle, and mandible, are formed directly from mesenchymal tissue. This type of ossification does not involve a cartilage precursor. The steps involved in intramembranous ossification include:
1. **Mesenchymal Cell Aggregation**: Mesenchymal cells aggregate and differentiate into osteoblasts, the bone-forming cells. 2. **Osteoid Formation**: Osteoblasts secrete osteoid, an unmineralized bone matrix composed primarily of collagen. 3. **Mineralization**: The osteoid becomes mineralized with calcium phosphate, forming woven bone. 4. **Bone Remodeling**: Woven bone is remodeled into lamellar bone, which is stronger and more organized.
Endochondral Ossification
Endochondral ossification is the process by which long bones and most other bones in the body are formed from a cartilage template. This type of ossification involves the replacement of hyaline cartilage with bone. The stages of endochondral ossification include:
1. **Cartilage Model Formation**: Mesenchymal cells differentiate into chondrocytes, which form a cartilage model of the bone. 2. **Primary Ossification Center Development**: Blood vessels invade the cartilage model, bringing osteoblasts that begin to replace cartilage with bone in the diaphysis. 3. **Secondary Ossification Centers**: These develop in the epiphyses of the bone, leading to the formation of the epiphyseal plates. 4. **Growth Plate Activity**: The epiphyseal plates allow for longitudinal growth of the bone until they close during puberty.
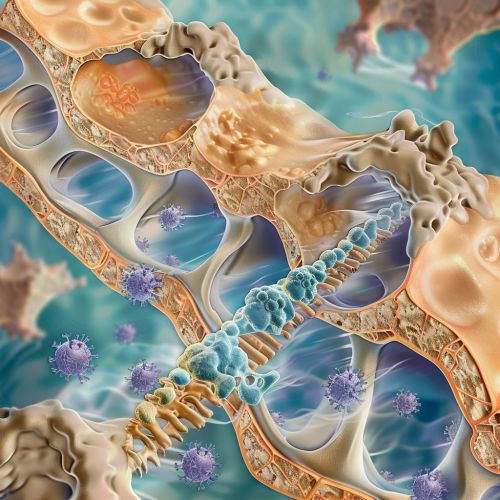
Cellular and Molecular Mechanisms
The process of ossification is regulated by a variety of cellular and molecular mechanisms. Key players in these processes include:
Osteoblasts
Osteoblasts are specialized cells responsible for bone formation. They originate from mesenchymal stem cells and produce the bone matrix, which consists of collagen and other proteins. Osteoblasts also play a crucial role in the mineralization of the bone matrix by secreting enzymes that facilitate the deposition of calcium and phosphate.
Osteoclasts
Osteoclasts are large, multinucleated cells derived from hematopoietic stem cells. They are responsible for bone resorption, a process that involves the breakdown of bone tissue. Osteoclasts secrete acids and proteolytic enzymes that dissolve the mineralized matrix and degrade collagen fibers. This activity is essential for bone remodeling and the maintenance of bone health.
Growth Factors and Cytokines
Several growth factors and cytokines regulate ossification, including:
- **Bone Morphogenetic Proteins (BMPs)**: These proteins are critical for the differentiation of mesenchymal cells into osteoblasts and chondrocytes.
- **Transforming Growth Factor-Beta (TGF-β)**: This cytokine regulates the proliferation and differentiation of osteoblasts and chondrocytes.
- **Insulin-like Growth Factors (IGFs)**: These factors promote the proliferation and differentiation of osteoblasts.
- **Fibroblast Growth Factors (FGFs)**: These proteins are involved in the proliferation and differentiation of chondrocytes during endochondral ossification.
Pathological Conditions
Several pathological conditions can affect the process of ossification, leading to abnormal bone formation or bone loss. Some of these conditions include:
Osteoporosis
Osteoporosis is a condition characterized by decreased bone mass and increased bone fragility. It occurs when the rate of bone resorption by osteoclasts exceeds the rate of bone formation by osteoblasts. This imbalance leads to weakened bones that are more susceptible to fractures.
Osteopetrosis
Osteopetrosis, also known as "marble bone disease," is a rare genetic disorder characterized by the abnormal hardening of bones. This condition results from defective osteoclast function, leading to impaired bone resorption and excessive bone formation. The bones become overly dense and brittle, making them prone to fractures.
Rickets and Osteomalacia
Rickets (in children) and osteomalacia (in adults) are conditions caused by a deficiency in vitamin D, calcium, or phosphate. These deficiencies lead to impaired mineralization of the bone matrix, resulting in soft and weak bones. Rickets is characterized by skeletal deformities, while osteomalacia presents with bone pain and muscle weakness.
Clinical Applications
Understanding the process of ossification has significant clinical implications. Advances in this field have led to the development of various therapeutic strategies for bone-related disorders.
Bone Grafting
Bone grafting is a surgical procedure used to repair or replace damaged or missing bone tissue. It involves the transplantation of bone tissue from a donor site to the affected area. Bone grafts can be autografts (from the patient's own body), allografts (from a donor), or synthetic materials. The success of bone grafting relies on the principles of ossification to promote the integration and regeneration of the grafted tissue.
Bone Tissue Engineering
Bone tissue engineering is an emerging field that aims to develop bioengineered bone constructs for the treatment of bone defects and injuries. This approach involves the use of scaffolds, growth factors, and stem cells to promote bone regeneration. The scaffolds provide a structural framework for cell attachment and proliferation, while growth factors and stem cells enhance the process of ossification.
