Neurobiology of depression
Introduction
Depression, a common and serious mood disorder, has been the subject of extensive scientific research. The neurobiological mechanisms underlying depression are complex and involve multiple brain regions and neural circuits. This article will delve into the neurobiology of depression, exploring the various biological factors that contribute to the development and persistence of this disorder.
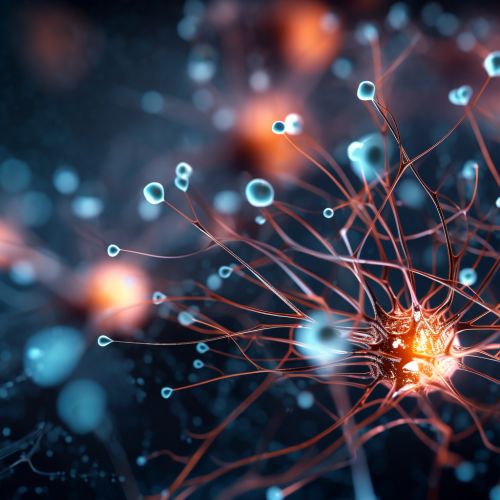
Neurotransmitters and Depression
Neurotransmitters, the chemical messengers of the brain, play a crucial role in mood regulation. Imbalances in neurotransmitters, particularly serotonin, norepinephrine, and dopamine, have been implicated in depression.
Serotonin, also known as 5-hydroxytryptamine (5-HT), is involved in regulating mood, appetite, and sleep. Reduced levels of serotonin in the brain have been associated with depressive symptoms. Antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs), work by increasing the availability of serotonin in the brain.
Norepinephrine is involved in the body's stress response. It is believed that low levels of norepinephrine in certain areas of the brain may contribute to the symptoms of depression.
Dopamine, the 'reward' neurotransmitter, is associated with pleasure and reward. Dysfunction in the dopamine system may lead to anhedonia, a core symptom of depression characterized by a lack of pleasure or interest in previously enjoyable activities.
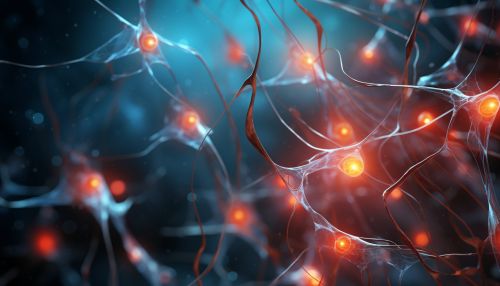
Neural Circuits and Depression
Depression is associated with dysfunction in several neural circuits, including the limbic-cortical-striatal-pallidal-thalamic circuit (LCSPTC). The LCSPTC is involved in mood regulation and emotional processing. Abnormalities in this circuit, particularly in the prefrontal cortex, amygdala, and hippocampus, have been linked to depression.
The prefrontal cortex (PFC) is involved in executive functions such as decision-making, problem-solving, and emotion regulation. Reduced activity in the PFC has been observed in individuals with depression.
The amygdala is involved in emotional processing and fear response. Hyperactivity of the amygdala has been associated with depression, particularly in response to negative stimuli.
The hippocampus is involved in memory formation and stress regulation. Reduced hippocampal volume has been observed in individuals with chronic depression, possibly due to prolonged exposure to stress hormones.
Genetic Factors
Depression has a significant genetic component, with heritability estimates ranging from 30% to 40%. Several genes have been implicated in depression, including those involved in the regulation of serotonin, norepinephrine, and dopamine, as well as genes involved in the body's stress response.
Hormonal Factors
Hormonal imbalances, particularly those involving cortisol and thyroid hormones, have been associated with depression. Chronic stress can lead to overactivity of the hypothalamic-pituitary-adrenal (HPA) axis, resulting in elevated levels of cortisol, the body's main stress hormone. Prolonged exposure to high levels of cortisol can lead to changes in brain structure and function, contributing to the development of depression.
Thyroid hormones are involved in many bodily functions, including mood regulation. Both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) have been associated with depressive symptoms.
Inflammation and Depression
Recent research suggests that inflammation may play a role in depression. Elevated levels of pro-inflammatory cytokines, proteins that regulate the body's immune response, have been observed in individuals with depression. It is believed that these cytokines can affect brain function, leading to depressive symptoms.

Treatment Implications
Understanding the neurobiology of depression can inform the development of more effective treatments. Current treatments for depression primarily target neurotransmitter imbalances, but these treatments are not effective for all individuals. Research into the role of neural circuits, genetic factors, hormonal imbalances, and inflammation in depression may lead to the development of novel treatments that target these underlying biological factors.
