Infective Endocarditis
Infective Endocarditis

Introduction
Infective endocarditis (IE) is a serious condition characterized by the infection of the endocardial surface of the heart, which includes the heart valves. This infection is typically caused by bacteria, but fungi and other microorganisms can also be responsible. The condition can lead to severe complications, including heart failure, systemic embolism, and death if not promptly diagnosed and treated.
Etiology
The primary causative agents of infective endocarditis are bacteria, with Staphylococcus aureus and Streptococcus viridans being the most common pathogens. Other notable bacteria include Enterococcus faecalis, Pseudomonas aeruginosa, and Haemophilus species. Fungal endocarditis, although less common, is often caused by Candida and Aspergillus species.
Risk factors for developing IE include pre-existing heart conditions such as rheumatic heart disease, congenital heart defects, and prosthetic heart valves. Intravenous drug use, poor dental hygiene, and invasive medical procedures can also increase the risk of infection.
Pathophysiology
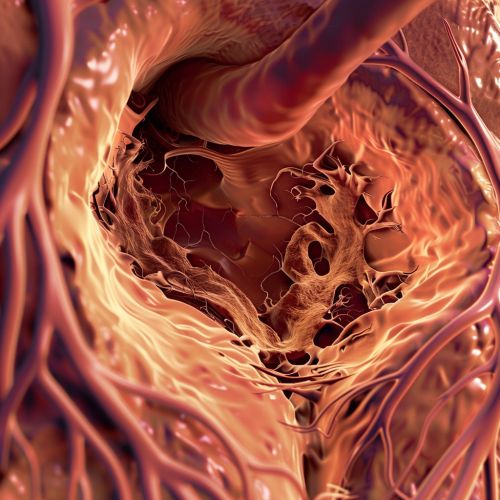
The pathogenesis of infective endocarditis involves the colonization of the endocardial surface by microorganisms. This process typically begins with the formation of a sterile thrombus on the endocardium, which serves as a nidus for microbial attachment. Once microorganisms adhere to the thrombus, they proliferate and form vegetations, which are masses of fibrin, platelets, and microorganisms.
These vegetations can cause local tissue destruction and can embolize, leading to systemic complications. The immune response to the infection can also result in immune complex deposition and vasculitis.
Clinical Manifestations
The clinical presentation of infective endocarditis can be highly variable, ranging from acute, rapidly progressive disease to a more indolent, subacute course. Common symptoms include fever, chills, night sweats, fatigue, and weight loss. Cardiac manifestations may include new or changing heart murmurs, heart failure, and arrhythmias.
Peripheral manifestations of IE include Janeway lesions, Osler nodes, Roth spots, and splinter hemorrhages. These findings are the result of embolic phenomena and immune complex deposition.
Diagnosis
The diagnosis of infective endocarditis is based on clinical criteria, blood cultures, and echocardiography. The Duke criteria are commonly used to establish the diagnosis, which includes major and minor criteria such as positive blood cultures, evidence of endocardial involvement on echocardiography, and the presence of predisposing heart conditions or intravenous drug use.
Blood cultures are essential for identifying the causative organism and guiding antibiotic therapy. Echocardiography, particularly transesophageal echocardiography (TEE), is crucial for detecting vegetations, abscesses, and other complications.
Treatment
The treatment of infective endocarditis involves prolonged courses of intravenous antibiotics tailored to the identified pathogen. Empirical therapy often includes a combination of antibiotics such as vancomycin and gentamicin until culture results are available.
Surgical intervention may be necessary in cases of heart failure, persistent infection despite appropriate antibiotic therapy, large vegetations, or embolic events. Valve replacement or repair is often required in these situations.
Complications
Infective endocarditis can lead to numerous complications, both cardiac and extracardiac. Cardiac complications include heart failure, valvular insufficiency, myocardial abscesses, and conduction abnormalities. Systemic embolization can result in stroke, pulmonary embolism, and infarctions of various organs.
Other complications include metastatic infections such as osteomyelitis, septic arthritis, and splenic abscesses. Immune-mediated phenomena such as glomerulonephritis and vasculitis can also occur.
Prevention
Preventive measures for infective endocarditis include maintaining good oral hygiene and regular dental care to reduce the risk of bacteremia from oral sources. Prophylactic antibiotics are recommended for high-risk individuals undergoing certain dental or surgical procedures.
High-risk individuals include those with prosthetic heart valves, previous history of infective endocarditis, certain congenital heart defects, and heart transplant recipients with valvulopathy.
Prognosis
The prognosis of infective endocarditis depends on several factors, including the causative organism, the presence of complications, and the timeliness of diagnosis and treatment. With appropriate therapy, the mortality rate has decreased, but it remains a serious condition with significant morbidity and mortality.
