Hyperacute Rejection
Overview
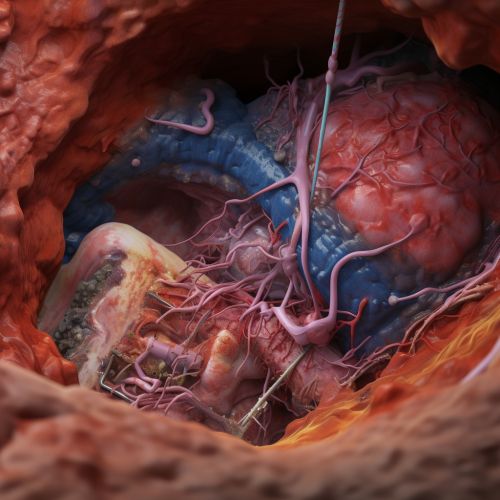
Hyperacute rejection is a form of transplant rejection that occurs within minutes to hours after transplantation. It is characterized by the rapid destruction of the graft tissue due to pre-existing antibodies in the recipient's blood that are directed against the donor's antigens. This type of rejection is most commonly seen in kidney transplants, but can occur in any type of organ transplant Organ Transplantation.
Pathophysiology
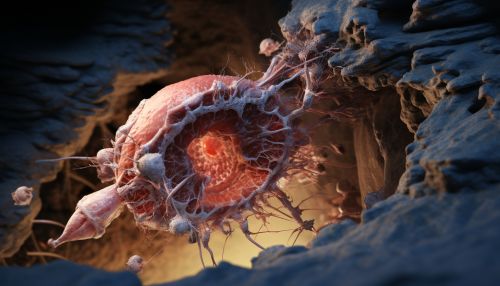
The pathophysiology of hyperacute rejection involves a type II hypersensitivity reaction. This is an immune response where antibodies bind to antigens on the surface of the transplanted cells, leading to their destruction. The antibodies involved are usually immunoglobulin G (IgG) and immunoglobulin M (IgM), which are produced by B cells in response to previous exposure to the donor's antigens. This could be due to a previous transplant, blood transfusion, or pregnancy.
When the antibodies bind to the antigens on the graft tissue, they activate the complement system, a part of the immune system that enhances the ability of antibodies to clear pathogens and damaged cells. The activation of the complement system leads to the formation of a membrane attack complex, which causes cell lysis and death. This results in the rapid destruction of the graft tissue.
Clinical Features
The clinical features of hyperacute rejection are usually immediate and dramatic. The transplanted organ becomes swollen and dark, and fails to function. In the case of a kidney transplant, there is immediate oliguria or anuria, indicating a lack of urine production. This is accompanied by pain at the site of the transplant.
Diagnosis
The diagnosis of hyperacute rejection is usually made based on the clinical features and the patient's history. Laboratory tests may show a rise in serum creatinine in kidney transplant patients, indicating a decline in kidney function. A biopsy of the graft tissue can confirm the diagnosis, showing widespread thrombosis and necrosis of the tissue.
Prevention and Treatment
The best way to prevent hyperacute rejection is through careful matching of the donor and recipient. This involves testing for the presence of pre-existing antibodies in the recipient's blood that are directed against the donor's antigens. This is done using a crossmatch test, which involves mixing the recipient's serum with the donor's lymphocytes. If the serum contains antibodies against the donor's antigens, they will bind to the lymphocytes and cause them to clump together, indicating a positive result.
If hyperacute rejection occurs, the only treatment is immediate removal of the graft. There are currently no effective treatments to reverse the process once it has started.
