Chronic Myeloid Leukemia
Introduction
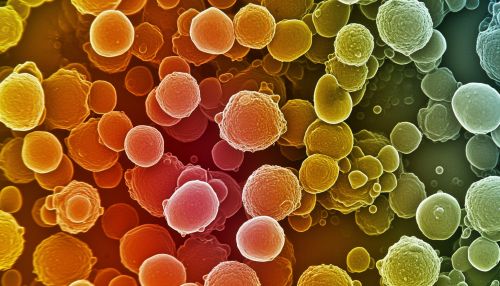
Chronic Myeloid Leukemia (CML) is a type of cancer that starts in certain blood-forming cells of the bone marrow. It is a form of leukemia characterized by the increased and unregulated growth of predominantly myeloid cells in the bone marrow and the accumulation of these cells in the blood.

Pathophysiology
CML is associated with a characteristic chromosomal translocation known as the Philadelphia (Ph) chromosome. This results from a reciprocal translocation between chromosome 9 and 22, t(9;22)(q34;q11), which forms a BCR-ABL1 fusion gene. The BCR-ABL1 fusion gene encodes for a protein with constitutive tyrosine kinase activity, which leads to increased cell proliferation and reduced DNA repair, causing the disease.
Epidemiology
CML represents approximately 15% of newly diagnosed cases of leukemia in adults. The incidence of CML increases with age, and it is slightly more common in males than in females. The median age at diagnosis is around 64 years.
Clinical Features
Patients with CML may present with a variety of symptoms. These can include fatigue, weight loss, night sweats, and a feeling of fullness in the left upper abdomen due to an enlarged spleen. Some patients may be asymptomatic and are diagnosed incidentally on a routine blood test.
Diagnosis
The diagnosis of CML is often suspected based on abnormal findings on a complete blood count (CBC), but definitive diagnosis requires confirmation of the Ph chromosome or BCR-ABL1 fusion gene. This is typically achieved through cytogenetic analysis, fluorescence in situ hybridization (FISH), or polymerase chain reaction (PCR).
Treatment
The treatment of CML has been revolutionized by the development of tyrosine kinase inhibitors (TKIs), such as imatinib. These drugs target the BCR-ABL1 fusion protein and have dramatically improved the prognosis for patients with CML. Other treatment options can include interferon-alpha, hydroxyurea, and stem cell transplantation.
Prognosis
The prognosis for patients with CML has significantly improved with the advent of TKIs. The overall survival rate at 5 years is now over 90%. However, some patients may develop resistance to TKIs, and this remains a challenge in the treatment of CML.
