Chorioamnionitis
Overview
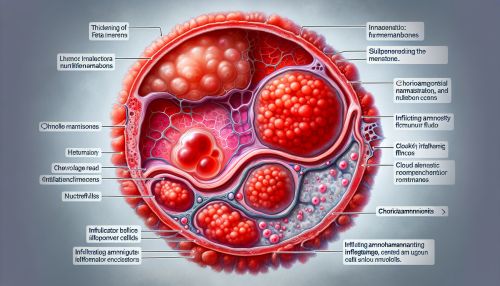
Chorioamnionitis, also known as intra-amniotic infection (IAI), is an inflammation of the fetal membranes (amnion and chorion) due to a bacterial infection. It typically results from bacteria ascending into the uterus from the vagina and is most often associated with prolonged labor. The condition is a significant contributor to maternal, perinatal, and long-term neonatal morbidity and mortality.

Etiology
The most common organisms associated with chorioamnionitis are Ureaplasma urealyticum, Mycoplasma hominis, Gardnerella vaginalis, and anaerobic bacteria including Bacteroides species. Less commonly, the condition can be caused by Group B streptococci, Escherichia coli, and other gram-negative rods.
Pathophysiology
In chorioamnionitis, bacteria ascend from the lower genital tract into the amniotic cavity, leading to an inflammatory response in the fetal membranes and amniotic fluid. This inflammation can lead to premature rupture of membranes (PROM) and preterm labor. If the infection progresses, it can result in bacteremia and maternal sepsis, a severe and potentially life-threatening condition.
Clinical Features
Chorioamnionitis typically presents with fever, uterine tenderness, maternal and fetal tachycardia, and purulent or foul-smelling amniotic fluid or vaginal discharge. However, clinical presentation can vary widely, and the condition can sometimes be asymptomatic or present with non-specific symptoms.
Diagnosis
Diagnosis of chorioamnionitis is typically clinical, based on the presence of maternal fever and at least one or two other signs such as uterine tenderness, malodorous vaginal discharge, maternal leukocytosis, or fetal tachycardia. Laboratory tests, including white blood cell count, C-reactive protein, and gram stain and culture of amniotic fluid, can also support the diagnosis.
Management
Management of chorioamnionitis involves antibiotics to treat the infection and measures to expedite delivery, given the risks of continued pregnancy in the context of intra-amniotic infection. Antibiotic regimens typically include a combination of ampicillin and gentamicin, with or without clindamycin.
Prognosis
The prognosis of chorioamnionitis depends on several factors, including the severity of the infection, the gestational age at which the infection occurs, and the promptness and effectiveness of treatment. With appropriate management, the prognosis is generally good, but the condition can have serious complications if not treated promptly and effectively.
Complications
Potential complications of chorioamnionitis include preterm birth, neonatal sepsis, neonatal pneumonia, cerebral palsy, and maternal sepsis. Long-term, children born to mothers with chorioamnionitis may have an increased risk of developmental delays and cognitive impairment.
Epidemiology
Chorioamnionitis affects approximately 1-4% of all pregnancies and is more common in preterm births, affecting up to 40-70% of preterm premature rupture of membranes (PPROM) cases.
Prevention
Prevention strategies for chorioamnionitis include screening and treatment for bacterial vaginosis in pregnancy, prophylactic antibiotics in women with PPROM, and limiting the number of vaginal examinations in labor, particularly in the presence of ruptured membranes.
