Bilirubin
Introduction
Bilirubin is a yellow compound that occurs in the normal catabolic pathway that breaks down heme in vertebrates. This catabolic pathway is crucial for the body's clearance of waste products that arise from the destruction of aged or abnormal red blood cells. Bilirubin is excreted in bile and urine, and elevated levels may indicate certain diseases. Understanding the biochemistry, physiology, and clinical significance of bilirubin is essential for medical professionals and researchers.
Biochemistry of Bilirubin
Structure and Formation
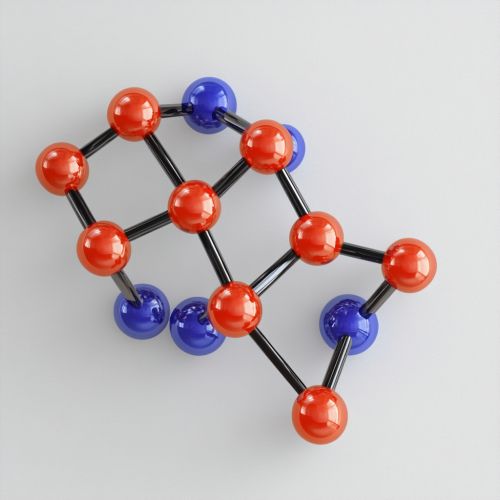
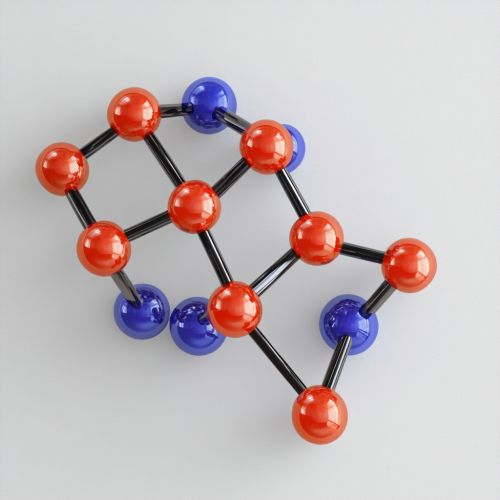
Bilirubin is a tetrapyrrolic bile pigment, which is a product of heme catabolism. The breakdown of heme is initiated by the enzyme heme oxygenase, which cleaves the heme ring to produce biliverdin, carbon monoxide, and free iron. Biliverdin is subsequently reduced to bilirubin by the enzyme biliverdin reductase. The chemical structure of bilirubin consists of two dipyrrolic subunits connected by a methylene bridge.
Types of Bilirubin
There are two main types of bilirubin: unconjugated (indirect) and conjugated (direct) bilirubin. Unconjugated bilirubin is lipid-soluble and is transported in the bloodstream bound to albumin. In the liver, it is conjugated with glucuronic acid by the enzyme UDP-glucuronosyltransferase, making it water-soluble. This conjugated bilirubin is then excreted into the bile and eventually into the small intestine.
Physiology of Bilirubin
Transport and Metabolism
Unconjugated bilirubin is transported to the liver bound to serum albumin. Once in the liver, it undergoes conjugation to form bilirubin diglucuronide, which is water-soluble. This conjugated bilirubin is secreted into the bile canaliculi and stored in the gallbladder or directly released into the small intestine. In the intestine, bacterial enzymes convert bilirubin into urobilinogen, some of which is reabsorbed and excreted by the kidneys, while the rest is converted to stercobilin and excreted in the feces.
Excretion
The excretion of bilirubin is a multi-step process involving the liver, bile ducts, intestines, and kidneys. Conjugated bilirubin is excreted into the bile and passes through the bile ducts into the duodenum. In the intestines, it is converted into urobilinogen by bacterial action. Urobilinogen can be reabsorbed into the bloodstream and excreted by the kidneys as urobilin, giving urine its characteristic yellow color. The remaining urobilinogen is converted to stercobilin and excreted in the feces, giving stool its brown color.
Clinical Significance
Hyperbilirubinemia
Hyperbilirubinemia is a condition characterized by elevated levels of bilirubin in the blood. It can be classified into unconjugated and conjugated hyperbilirubinemia. Unconjugated hyperbilirubinemia can result from increased production of bilirubin, decreased uptake by the liver, or impaired conjugation. Conjugated hyperbilirubinemia is usually due to impaired excretion of bilirubin from the liver or obstruction of the bile ducts.
Jaundice
Jaundice is a clinical manifestation of hyperbilirubinemia, characterized by yellowing of the skin, sclerae, and mucous membranes. It can be classified into pre-hepatic, hepatic, and post-hepatic jaundice based on the underlying cause. Pre-hepatic jaundice is due to excessive hemolysis, hepatic jaundice results from liver diseases such as hepatitis or cirrhosis, and post-hepatic jaundice is caused by obstruction of the bile ducts.
Diagnostic Tests
Several diagnostic tests are used to measure bilirubin levels and assess liver function. The total serum bilirubin test measures both conjugated and unconjugated bilirubin. The direct bilirubin test measures only conjugated bilirubin, while the indirect bilirubin test measures unconjugated bilirubin. Other liver function tests, such as alanine transaminase (ALT) and aspartate transaminase (AST), are often performed alongside bilirubin tests to diagnose liver diseases.
Pathophysiology
Hemolytic Anemia
Hemolytic anemia is a condition in which red blood cells are destroyed faster than they can be produced. This leads to increased production of bilirubin, resulting in unconjugated hyperbilirubinemia. Common causes of hemolytic anemia include autoimmune disorders, genetic conditions such as sickle cell disease, and infections.
Liver Diseases
Liver diseases such as hepatitis, cirrhosis, and liver cancer can impair the liver's ability to conjugate and excrete bilirubin, leading to hepatic jaundice. In hepatitis, inflammation of the liver cells disrupts bilirubin metabolism. Cirrhosis involves the replacement of healthy liver tissue with scar tissue, impairing liver function. Liver cancer can obstruct bile ducts, causing post-hepatic jaundice.
Biliary Obstruction
Biliary obstruction is a blockage of the bile ducts that prevents the normal flow of bile from the liver to the intestines. This can result from gallstones, tumors, or strictures. Biliary obstruction leads to conjugated hyperbilirubinemia and post-hepatic jaundice. Symptoms include dark urine, pale stools, and itching.
Treatment and Management
Phototherapy
Phototherapy is a common treatment for neonatal jaundice, a condition characterized by high levels of unconjugated bilirubin in newborns. Exposure to blue light converts bilirubin into water-soluble isomers that can be excreted without conjugation. This treatment is effective in reducing bilirubin levels and preventing kernicterus, a type of brain damage caused by excessive bilirubin.
Medications
Medications such as phenobarbital can induce the activity of UDP-glucuronosyltransferase, enhancing the conjugation and excretion of bilirubin. In cases of biliary obstruction, medications such as ursodeoxycholic acid can improve bile flow. Antioxidants and anti-inflammatory drugs may also be used to manage liver diseases and reduce bilirubin levels.
Surgical Interventions
Surgical interventions may be necessary in cases of biliary obstruction or liver tumors. Procedures such as cholecystectomy (removal of the gallbladder) or bile duct stenting can relieve obstruction and restore bile flow. Liver transplantation may be considered for patients with end-stage liver disease.
