Biliary Stents
Overview
A biliary stent is a tubular device made of plastic or metal, inserted into a bile duct to relieve obstruction. The bile ducts carry bile from the liver and gallbladder to the small intestine to aid in the digestion of fats. When these ducts become blocked, it can cause serious health complications, including jaundice and infection. Biliary stents are used to open up the blocked ducts and allow bile to flow freely again.
Indications for Use
Biliary stents are used in the management of various conditions that cause obstruction of the bile ducts. These include:
- Cholangiocarcinoma (bile duct cancer): This is a rare and often deadly type of cancer that forms in the bile ducts. A biliary stent can be used to relieve symptoms and improve quality of life in patients with this condition.
- Gallstones: These are hard deposits that form in the gallbladder and can block the bile ducts. If a gallstone cannot be removed through other methods, a biliary stent may be placed to allow bile to flow around the stone.
- Pancreatic cancer: This type of cancer can cause blockage of the bile ducts as it grows. A biliary stent can be used to relieve jaundice and other symptoms in these patients.
- Chronic pancreatitis: This is a long-term inflammation of the pancreas that can cause scarring and blockage of the bile ducts. A biliary stent can be used to manage this condition.
Types of Biliary Stents
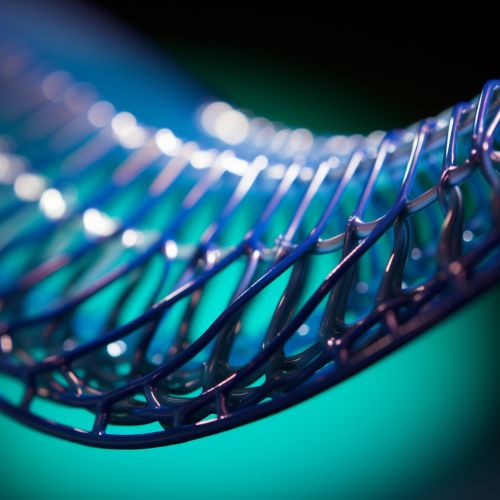
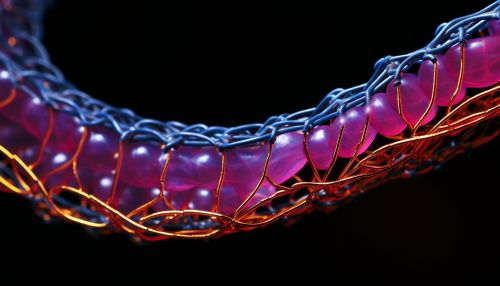
There are two main types of biliary stents: plastic stents and self-expanding metal stents (SEMS).
- Plastic stents: These are made of a flexible plastic material and are typically used for temporary relief of bile duct obstruction. They are less expensive than metal stents but need to be replaced more frequently, usually every 3 to 4 months.
- Self-expanding metal stents (SEMS): These are made of a metallic mesh that expands once it's placed in the bile duct. They are more durable and have a longer patency period than plastic stents, but are also more expensive.
Procedure
The procedure to place a biliary stent is typically performed by a gastroenterologist or a radiologist. The most common method is endoscopic retrograde cholangiopancreatography (ERCP), although percutaneous transhepatic cholangiography (PTC) can also be used.
- Endoscopic retrograde cholangiopancreatography (ERCP): In this procedure, an endoscope (a flexible tube with a light and camera at the end) is passed through the mouth, esophagus, and stomach into the first part of the small intestine. A smaller tube (catheter) is then inserted through the endoscope into the bile ducts. A dye is injected into the bile ducts and X-rays are taken to locate the blockage. Once the blockage is located, the stent is inserted through the catheter and positioned in the blocked area.
- Percutaneous transhepatic cholangiography (PTC): In this procedure, a thin needle is inserted through the skin and into the liver. A dye is injected and X-rays are taken to locate the blockage. The stent is then inserted through the needle and positioned in the blocked area.
Complications
While biliary stent placement is generally safe, complications can occur. These may include:
- Infection: This can occur if bacteria enter the bile ducts during the procedure.
- Stent migration: The stent can move from its original position, which may require another procedure to reposition or replace it.
- Stent occlusion: The stent can become blocked by bile sludge, tissue growth, or a blood clot.
- Cholecystitis: Inflammation of the gallbladder can occur if a stent blocks the cystic duct (the duct that connects the gallbladder to the common bile duct).
- Pancreatitis: Inflammation of the pancreas can occur as a complication of ERCP.
Future Developments
Research is ongoing to develop new types of biliary stents and improve the design of existing ones. This includes the development of drug-eluting stents, which release medication to prevent tissue growth and stent occlusion, and bioabsorbable stents, which dissolve over time and do not need to be removed.
