Acinetobacter baumannii
Introduction
Acinetobacter baumannii is a gram-negative, opportunistic pathogen that has become a significant concern in healthcare settings due to its multidrug-resistant (MDR) nature. This bacterium is known for causing a variety of infections, particularly in immunocompromised patients, and is notorious for its ability to survive in harsh environments, making it a formidable adversary in hospital-acquired infections.
Taxonomy and Classification
Acinetobacter baumannii belongs to the family Moraxellaceae, within the order Pseudomonadales. It is one of the most clinically relevant species within the genus Acinetobacter. The taxonomy of A. baumannii has undergone several revisions, and it is closely related to other species within the Acinetobacter calcoaceticus-baumannii complex (ACB complex), which includes A. calcoaceticus, A. pittii, and A. nosocomialis.
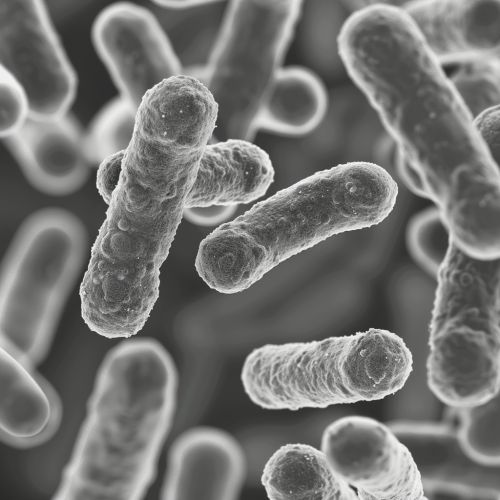
Morphology and Physiology
A. baumannii is a non-motile, non-fermentative, aerobic coccobacillus. It typically appears as short rods under the microscope and forms smooth, opaque colonies on agar plates. The bacterium is oxidase-negative and catalase-positive, a characteristic that aids in its identification in clinical laboratories.
Pathogenesis
A. baumannii is an opportunistic pathogen, primarily affecting individuals with compromised immune systems. It is known to cause a range of infections, including pneumonia, bacteremia, meningitis, urinary tract infections, and wound infections. The pathogenesis of A. baumannii involves several virulence factors:
Adhesion and Biofilm Formation
A. baumannii has the ability to adhere to various surfaces and form biofilms, which are structured communities of bacteria encased in a self-produced extracellular matrix. Biofilm formation enhances the bacterium's resistance to antibiotics and disinfectants, contributing to its persistence in hospital environments.
Iron Acquisition Systems
Iron is essential for bacterial growth and survival. A. baumannii possesses multiple iron acquisition systems, including siderophore-mediated uptake and heme utilization systems, which allow it to thrive in iron-limited environments such as the human body.
Outer Membrane Proteins and Lipopolysaccharides
The outer membrane of A. baumannii contains proteins and lipopolysaccharides (LPS) that play crucial roles in immune evasion and antibiotic resistance. The LPS can trigger a strong inflammatory response, contributing to the severity of infections.
Antibiotic Resistance
One of the most alarming features of A. baumannii is its ability to develop resistance to multiple antibiotics. The mechanisms of antibiotic resistance in A. baumannii are diverse and include:
Beta-Lactamases
A. baumannii produces various beta-lactamases, enzymes that hydrolyze beta-lactam antibiotics, rendering them ineffective. These include extended-spectrum beta-lactamases (ESBLs) and carbapenemases, which confer resistance to a broad range of beta-lactam antibiotics, including carbapenems.
Efflux Pumps
Efflux pumps are membrane proteins that actively expel antibiotics from the bacterial cell, reducing their intracellular concentrations and effectiveness. A. baumannii possesses several efflux pump systems, such as the AdeABC, AdeFGH, and AdeIJK systems, which contribute to its multidrug resistance.
Porin Alterations
Porins are channels in the outer membrane that allow the passage of small molecules, including antibiotics. Alterations or loss of porins in A. baumannii can decrease the uptake of antibiotics, contributing to resistance.
Target Site Modifications
A. baumannii can modify the target sites of antibiotics, such as the penicillin-binding proteins (PBPs) and ribosomal subunits, reducing the binding affinity of the drugs and rendering them ineffective.
Epidemiology
A. baumannii is a significant cause of hospital-acquired infections (HAIs), particularly in intensive care units (ICUs). The bacterium is capable of surviving on various surfaces for extended periods, facilitating its spread within healthcare settings. Outbreaks of A. baumannii infections are often associated with contaminated medical equipment, healthcare personnel, and environmental surfaces.
Diagnosis
The diagnosis of A. baumannii infections involves the isolation and identification of the bacterium from clinical specimens, such as blood, urine, cerebrospinal fluid, or wound swabs. Laboratory techniques used for identification include:
Culture and Biochemical Tests
A. baumannii can be cultured on standard bacteriological media, such as blood agar and MacConkey agar. Biochemical tests, such as oxidase and catalase tests, are used to differentiate A. baumannii from other gram-negative bacteria.
Molecular Methods
Polymerase chain reaction (PCR) and sequencing techniques are employed for the rapid and accurate identification of A. baumannii. These methods can also detect specific resistance genes and virulence factors.
Treatment
The treatment of A. baumannii infections is challenging due to its multidrug-resistant nature. The choice of antibiotics depends on the susceptibility profile of the isolate. Commonly used antibiotics include:
Carbapenems
Carbapenems, such as imipenem and meropenem, are often considered the drugs of choice for treating severe A. baumannii infections. However, the emergence of carbapenem-resistant strains has limited their effectiveness.
Polymyxins
Polymyxins, such as colistin and polymyxin B, are used as last-resort options for treating MDR A. baumannii infections. These antibiotics disrupt the bacterial cell membrane, leading to cell death.
Tigecycline
Tigecycline is a broad-spectrum antibiotic that is effective against many MDR bacteria, including A. baumannii. It is often used in combination with other antibiotics to enhance its efficacy.
Combination Therapy
Combination therapy, involving the use of two or more antibiotics with different mechanisms of action, is often employed to overcome resistance and achieve better clinical outcomes.
Prevention and Control
Preventing and controlling A. baumannii infections in healthcare settings require a multifaceted approach:
Infection Control Measures
Strict adherence to infection control measures, such as hand hygiene, the use of personal protective equipment (PPE), and environmental cleaning, is essential to prevent the spread of A. baumannii.
Antimicrobial Stewardship
Implementing antimicrobial stewardship programs to optimize the use of antibiotics and reduce the selection pressure for resistant strains is crucial in controlling the spread of MDR A. baumannii.
Surveillance
Regular surveillance of A. baumannii infections and resistance patterns helps in early detection and timely intervention to prevent outbreaks.
Research and Future Directions
Ongoing research on A. baumannii focuses on understanding its pathogenesis, resistance mechanisms, and developing new therapeutic strategies. Areas of interest include:
Novel Antimicrobials
The development of new antibiotics and alternative therapies, such as bacteriophage therapy and antimicrobial peptides, is being explored to combat MDR A. baumannii.
Vaccine Development
Research is underway to develop vaccines against A. baumannii to provide long-term protection and reduce the incidence of infections.
Genomic Studies
Genomic studies aim to elucidate the genetic basis of virulence and resistance in A. baumannii, providing insights into potential targets for novel therapeutics.